Late in May one afternoon, R Ramkumar, a 63-year-old resident of Madipakkam, felt seriously indisposed when he started experiencing mild dizziness without any warning signs. Hospitals were teeming with COVID patients at this time, and the family did not want to expose the senior citizen to unnecessary risk. After brief deliberation on the matter, they decided to go for teleconsultation with a doctor and did so through Practo, a medical portal that connects patients with doctors for meeting various healthcare needs.
Upon the doctor’s advice, the family did an instant blood glucose level test with the equipment available at home. It turned out that Ramkumar’s blood sugar levels had dropped, but he was stable and not critical. The doctor-on-call assessed him further and prescribed medicines for a week. Ramkumar was in regular touch with the doctor until his recovery which took about a week.
The COVID-19 pandemic has shone the spotlight on the crumbling national health infrastructure and highlighted the glaring gap in human resources in the medical sector. At the peak of COVID in Chennai, the increase in case load was hugely disproportionate to the manpower available at hospitals and the doctor-patient ratio was found to be around 1:30. In fact, in some hospitals, there was just one doctor for as many as 50 patients as the above report shows.
Thus, on one hand, doctors were stretched thin while on the other, outpatient services were either discontinued or patients were discouraged from physical visits to minimise spread. Under these circumstances, telemedicine or virtual consultations became the fall-back option for many non-COVID, non-critical patients in the city. But is this a trend that will outlive the health emergency created by the pandemic?
What is telemedicine?
First things first, what exactly is telemedicine?
According to the World Health Organization (WHO), telemedicine is defined as “The delivery of healthcare services, where distance is a critical factor, by all healthcare professionals using information and communications technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and the continuing education of healthcare workers, to advance the health of individuals and communities.”
Simply put, telemedicine is the use of technology to treat a patient remotely, when it is physically impossible for the doctor and patient to meet in person. This could involve consultations over normal phone calls, or video consultations, eventually leading to virtual evaluation, diagnosis, treatment or prevention.
Rise of telemedicine

A 2020 survey by Practo reveals that among the Indian metropolitan cities, Chennai witnessed the highest growth of 4x in teleconsultation cases, as compared to the previous year. Dr Vinod Rajkumar, an orthopaedic consultant, working in a government hospital who also practises independently, says he has been receiving double the amount of calls from patients that he usually does, seeking teleconsultation. “My private practice hours are very limited, I see about five patients at the maximum and spend around two hours consulting remotely over the phone every day,” he says. But is it feasible in every case?
“Although orthopaedics is a field that ideally requires in-person visits, teleconsultation helps to an extent when the case is not severe. I suggest my patients take an X-ray if they are in deep discomfort and ask them to send a picture of it for further diagnosis and treatment. As long as it does not involve surgery, teleconsultation can play a major role in connecting doctors with patients,” adds Dr Vinod.
Dr Srikanth Ramasubramanian, senior consultant, Opthalmology, Apollo Spectra, has observed similar trends. He receives about seven to ten patients via teleconsultation every day. Talking about it, he says, “Many of my patients are satisfied with teleconsultation and also refer others. This virtual model of consultation has helped a great deal to avoid physical consultation during the times of lockdown and avoiding unnecessary travel.”
Elaborating on the disadvantages, however, Srikanth says, “Sometimes the examination may not be complete or accurate in the absence of the equipment needed. For special fields like ophthalmology, using certain equipment may be mandatory for routine examinations. But some conditions like external eye lesions can be managed with teleconsultations too.”
Implementation of norms and challenges
With access to healthcare through teleconsultation picking up in the wake of the pandemic, the Medical Council of India (MCI) released detailed guidelines for doctors to practice telemedicine.
Read more: How GCC’s telemedicine services are helping manage this COVID wave
According to the guidelines, only Registered Medical Practitioners (RMPs) are entitled to provide telemedicine consultation to patients from any part of India. They should be familiar with the guidelines, the process and limitations of telemedicine practice. For this, the Medical Council of India (MCI) will develop an online course for healthcare practitioners.
The guidelines state that doctors intending to provide online consultation need to complete the mandatory online course within three years of its notification. While the course by MCI is yet to be rolled out, it is suggested that the principles mentioned in these guidelines need to be followed in the interim period. In view of this, private hospitals and some of the medical portals that facilitate teleconsultation are offering their own training modules or programmes for doctors. For example, the Telemedicine Society of India Tamilnadu Chapter (TSITN) has already trained around 1000 doctors from Chennai for teleconsultation.
Talking about the challenges in the implementation of norms, TSITN president, Dr Sunil Shroff says, “Many practitioners are unaware of the norm that calls for completion of a mandatory course. It is important to take the course as it sheds light on various nuances of teleconsultation, including seeking consent from patients, safeguarding patient details and the likes.”
One of the other major challenges in teleconsultation relates to maintaining data privacy. The norms state that the RMP should take absolute care to safeguard patient data as per the Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulations, 2002 and under the relevant provisions of the IT Act, Data protection and privacy laws, or any applicable rules notified from time to time for protecting patient privacy and confidentiality. The RMP will not be held responsible for data breach, if there is reasonable evidence to believe that a patient’s privacy and confidentiality has been compromised by technology or by a third person other than the RMP.
These clauses are crucial given the fact that doctors must seek basic details including age and gender and information on other health conditions from the patient if they are to treat them. Other forms of data that can be stored on the devices used for teleconsultation are logs or records of teleconsultation, patient-specific data like diagnostic reports, images etc and prescription details. The data could be stored in different formats (hard copies and digital formats). The threat of confidentiality breach becomes higher when sensitive information is stored in digital format, where third party applications are used.
“Doctors should use personalised applications or credible tools created by verified developers like Practo, DocOn, Lybrate and Apollo. They must also go through the privacy policy of the applications to safeguard the patient data,” adds Vinod.
Prescriptions on teleconsultation
The MCI has also released guidelines pertaining to the medicines that can be prescribed. According to the regulations, there are four categories of medicines which are as follows:
- List O: These are medicines safe to be prescribed through any mode of teleconsultation. In essence, they would comprise ‘over the counter’ medications.
- List A: These medications are those which can be prescribed following a first video consultation, and can be re-prescribed (for refill) in case of follow-up. This would be an inclusion list, containing relatively safe medicines with low potential for abuse.
- List B: It is a list of medications which an RMP can prescribe in a patient who is undergoing follow-up consultation, in addition to those which have been prescribed during an in-person consult for the same medical condition.
- Prohibited List: An RMP providing consultation via telemedicine cannot prescribe medicines in this list as these medicines have a high potential of abuse and could harm the patient or the society at large if used improperly. These include medicines listed in Schedule X of Drug and Cosmetic Act and Rules or any Narcotic and Psychotropic substance listed in the Narcotic Drugs and Psychotropic Substances, Act, 1985.
How to make a teleconsultation session successful
Dr Vinod and Dr Srikanth have some important pointers for patients on how to make the best use of virtual consultations.
- Patients should keep their questions prepared
- Old prescriptions should be kept handy
- Write down all the queries before the consultation and clarify doubts during the consultation
- It is important to have a stable Internet connection and a good camera
- Do not hesitate to call the doctor immediately in case of patients developing any allergy or other symptoms during the course of treatment
Importance of paramedical care
Nursing, physiotherapy and home patient care are some of the crucial paramedical services that certain sections of patients might need, even after diagnosis through teleconsultation. While virtual consultations can be handy, paramedical care is an aspect that cannot be ignored.
“In Chennai, you can get physiotherapists to come home for the therapy. Similarly, remote diagnostic facilities have also improved tremendously, labs depute technicians for home collection of samples. However, we do not have sufficient number of nurses and home patient care attendants to tend to patients who are bed-ridden,” says Dr K Kolandaswamy, former director of Tamil Nadu Department of Public Health & Family Welfare.
Access and acceptance
The other question that arises over teleconsultation as a healthcare solution is about inclusion, given that it mostly caters to the needs of people who have access to devices with Internet connection.
Dr Kolandaswamy feels that it has become possible to overcome digital barriers to a significant extent. “Firstly, the scope of telemedicine is limited at present. Secondly, a simple voice call that does not require smartphones can also be used for teleconsultation. The helplines launched by the state and city governments are inclusive and enable people to consult a doctor even if they do not have Internet or a smartphone. Where the patient’s health condition is complicated, they should in any case opt for an in-person consultation,” he says.
Dr Sunil Shroff of TSITN too feels that telemedicine has got huge potential, especially with the Union government showing interest in tapping the advantages of telemedicine, “It is affordable and considered a time-saver for patients. Teleconsultations are here to stay even after the pandemic,” he adds.
“Primary Healthcare Centres (PHCs) or Amma Mini Clinics in the city do not function 24*7 and there are also reports of the centres being closed all through the day. In such cases, telephonic or virtual consultations for minor health conditions such as fever, cold and cough could well be the way forward for primary health care,” says Dr R Anandi, a general practitioner from a city-based government hospital.
While doctors see teleconsultation as an opportunity to reduce the burden on the existing healthcare system and even a potential long term trend, it is also important to understand what patients feel or expect from virtual consultations. R Sunanda, a 65-year-old resident with hypertension from Kellys, had opted for teleconsultation with a doctor at the private hospital in her neighbourhood. She had severe joint pain at the time. From her experience, she says, “It cannot be an alternative to in-person visits, as virtual modes do not really offer the time that a patient needs to get accustomed to doctors. This is also essential for the build-up of empathy, so crucial to the efficacy of treatment. Secondly, the chances of misdiagnosis are high if the patient cannot communicate his/her symptoms properly or if the doctor lacks experience.”
Dr Srikanth believes that while remote medical consultations cannot replace physical consultations, they can certainly supplement regular consultations. “There is scope for a lot of growth in teleconsultation and with time its accuracy in diagnosis will also improve. With advancements in use and application of artificial intelligence, the scope for teleconsultations will increase further,” he states.
Establishing credibility
The regulations make it mandatory for an RMP to begin his/her consultation by informing the patient about his/her name and qualifications. Every RMP should display the registration number accorded to him/her by the State Medical Council/MCI, on prescriptions, website, electronic communication (WhatsApp/ email etc.) and receipts etc. given to his/her patients.
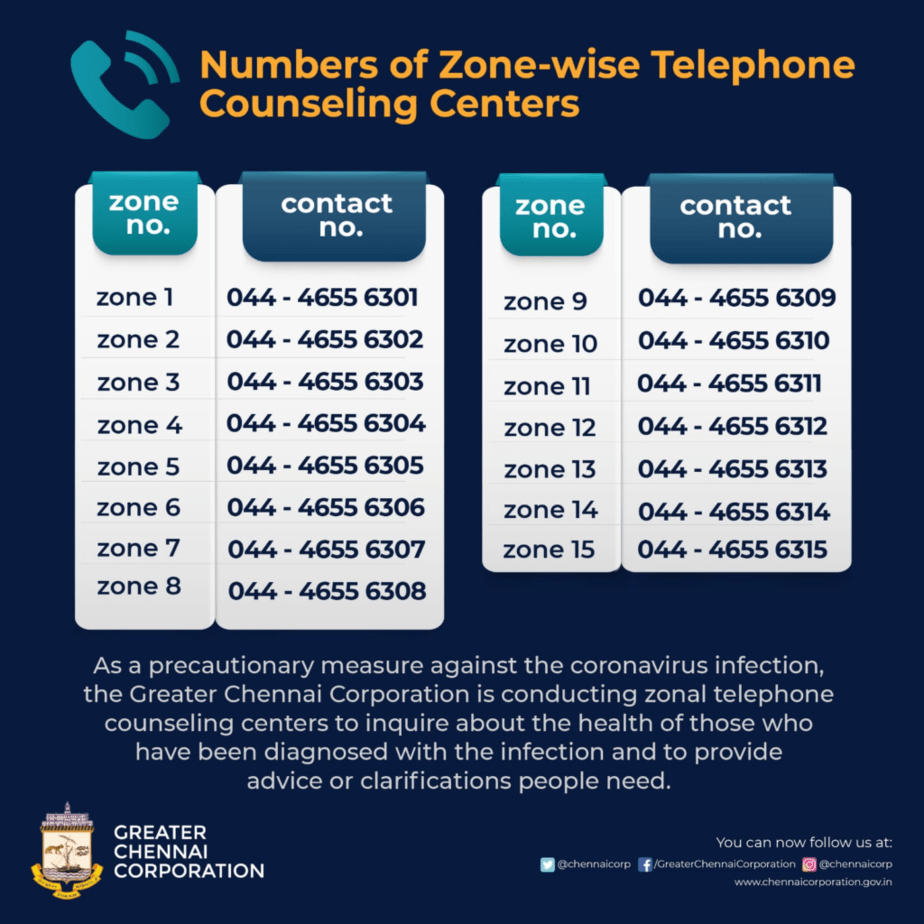
The Greater Chennai Corporation has initiated telemedicine services. Here is the zone-wise list of helplines. The VIDMED application rolled out by the civic body also offers teleconsultation. Besides this, the Tamil Nadu chapter of Telemedicine Society of India is also offering telemedicine services.