In mid-May, R Shanthi, a resident of CIT Nagar, tested positive for COVID-19 and isolated herself at home. In her 50s, Shanthi had mild symptoms that included fever and cough. It was a time of great anxiety and stress, but what kept her reassured to an extent were the phone calls that she received every second day, from the doctor deputed at Chennai Corporation’s zonal telemedicine department. Telemedicine has indeed been a boon for many patients like Shanthi battling the virus at home.
Ever since the pandemic took centre stage, access to medical consultation for both COVID and non-COVID patients has been a challenge with the entire healthcare system stretched to its limits. In Chennai, the doctor-patient ratio is 1:30 that underlines the need for teleservices or remote consultations during health crises of such proportions as we see in the present.
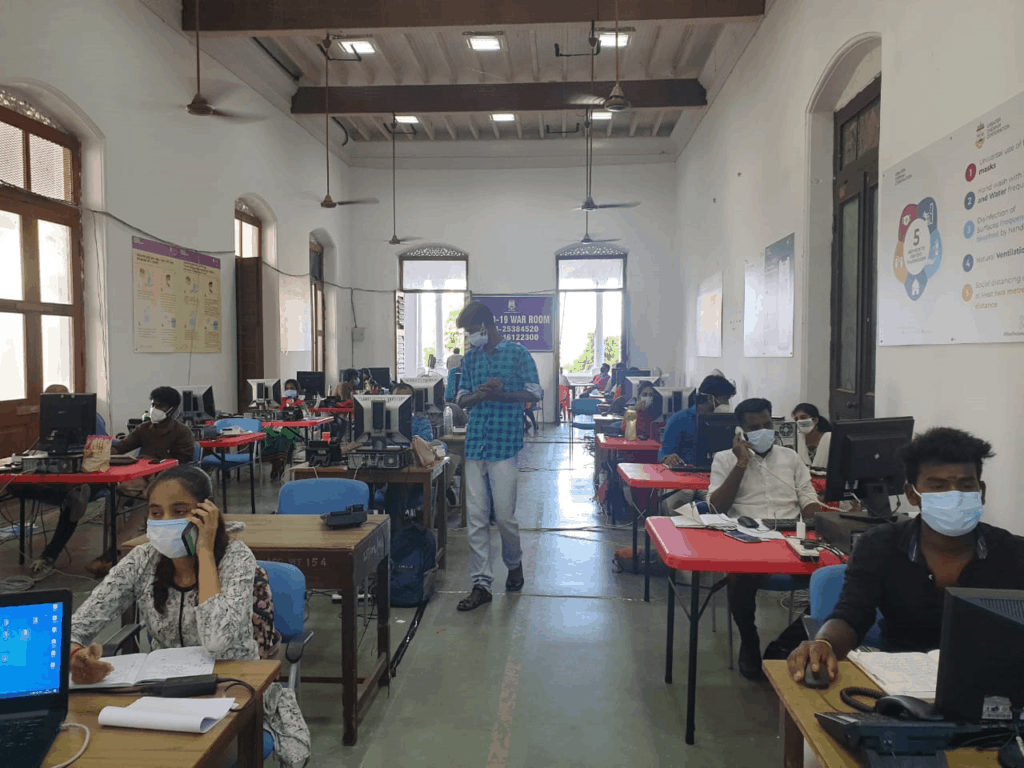
Recognising the shortage of healthcare workers in the face of the rising number of COVID cases during the first wave last year, the Greater Chennai Corporation (GCC) launched a telemedicine department in March 2020, to ensure that even patients at home could have their medical needs attended to. As the second wave raged on and COVID numbers exploded in the city, the civic body appointed 300 pre-final-year medical students as trainee medical officers at the telemedicine “war room” and across zonal centres to meet various needs.
The centre has come a long way since it started functioning last year. Following up on patients for symptoms, referrals for testing, providing psychosocial support to callers in need, professional counselling, admission coordination with hospitals, coordination of relief for the needy, contact tracing through calls and data records are some of the tasks within the wide range of functions that people working in the telemedicine centre currently perform. “The volunteers working in this project undergo intensive training for tracking symptoms, triaging and vaccination,” explains Dr Pradeep Selvaraj, District Programme Officer (NCD), who is monitoring the teleservices of GCC.
Read more: Supporting COVID patients in isolation: Chennai apartment sets example
Learnings from the first wave
At the peak of the COVID curve in the first wave, a teleconsultation wing was initiated at Amma Maligai by the Greater Chennai Corporation, which was functional for about six months. It had five doctors working in one shift and received around 70 calls per day.
“Back then we categorised COVID patients into two categories — patients in home isolation and people admitted to the COVID Care Centres, who could turn serious. We were assigned to call up these patients to enquire about their general condition and ensure that medicines were being delivered and administered,” explains Dr M Balakrishnan, who was in the telemedicine wing last year.
Besides teleservices, the Corporation also launched the GCC VIDMED application for people who would like to avail a video call consultation with doctors.
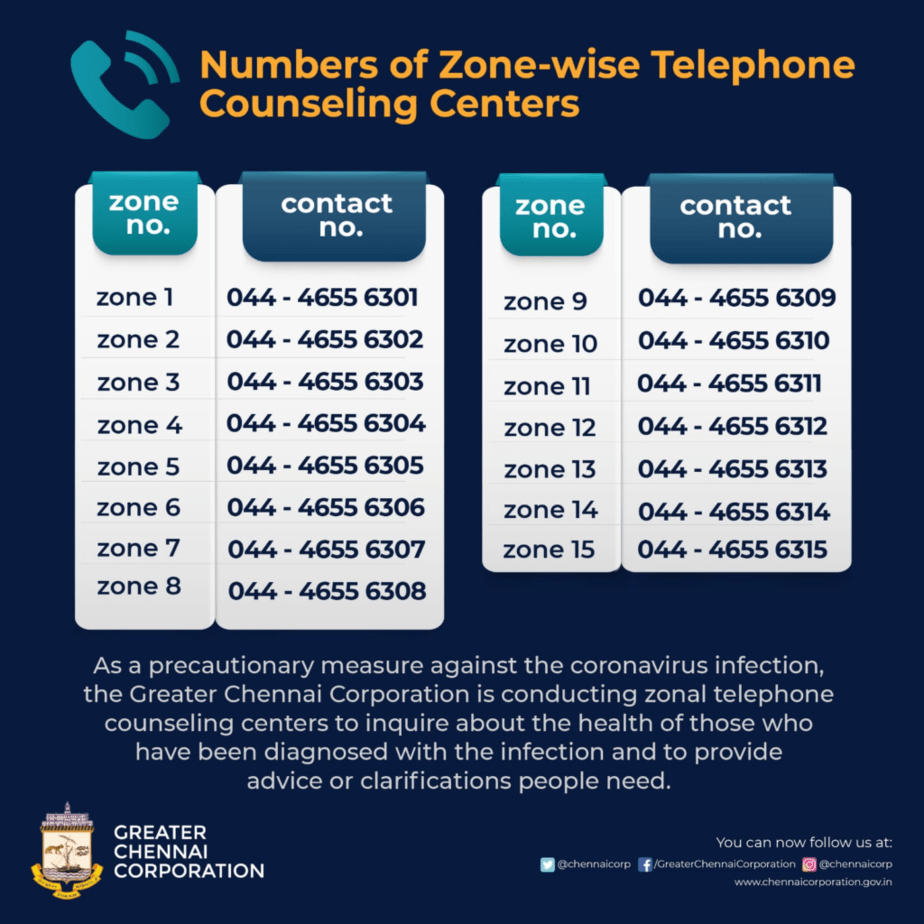
As the number of new cases dipped towards the end of 2020, teleservices were discontinued. But with the second wave, cases peaked again so that the civic body restarted the service. As part of the efforts, the Corporation also set up a 24*7 war-room and a tele-counseling centre at the Ripon Building and Amma Maligai, respectively. To meet the increasing demand for teleservices, the corporation expanded it into a hub and spoke model by setting up telemedicine centres at the 15 zones of the corporation and deputing trainee medical officers in each.
Round-the-clock war-room
While the tele-counseling team keeps a tab on home-isolated patients, the war-room handles the COVID helplines. Depending on the kinds of medical needs, the war-room redirects the calls to zonal telemedicine centres or the triaging departments which also function from Ripon Building.
There are about 25 to 50 non-doctor volunteers working in each shift at the tele counseling centre. Their work involves tracking patients who have been isolated at home for a long period, calling them every day and offerring psychological support. The department works in two shifts: 7 am to 3 pm and 2 pm to 10 pm.
The war room at the Ripon building handles the COVID helplines — 044 4612 2300 and 044 2538 4520 and 1913. The team has 25-30 non-doctor volunteers and functions in three shifts (7 am to 3 pm, 2 pm to 10 pm and 1 pm to 7 am). Depending on the request of the caller, the call is diverted to the respective centres.
“If the patient requires psycho-social support, we connect them to the tele-counselling team and in case they need an appointment with a doctor, we reroute the call to the VIDMED team,” explains Dr Pavithra Jayakumar, Trainee Medical Officer.
Read more: Not just a supply crunch: The real reason why patients in need of oxygen are suffering
One can use a mobile app to connect with the VIDMED team, but they also have a landline and mobile phones for attending to regular calls. This ensures that the needs of people who do not have access to the Internet is also met. “Everyone may not have a mobile phone or an Internet connection; to ensure every need is met, we offer all possible options,” adds Pavithra.
The VIDMED team has 5 to 7 doctors working in three shifts. On an average, every doctor gets about 25-30 calls. While 90% of the queries are related to COVID, 10% account for non-COVID medical consultations.
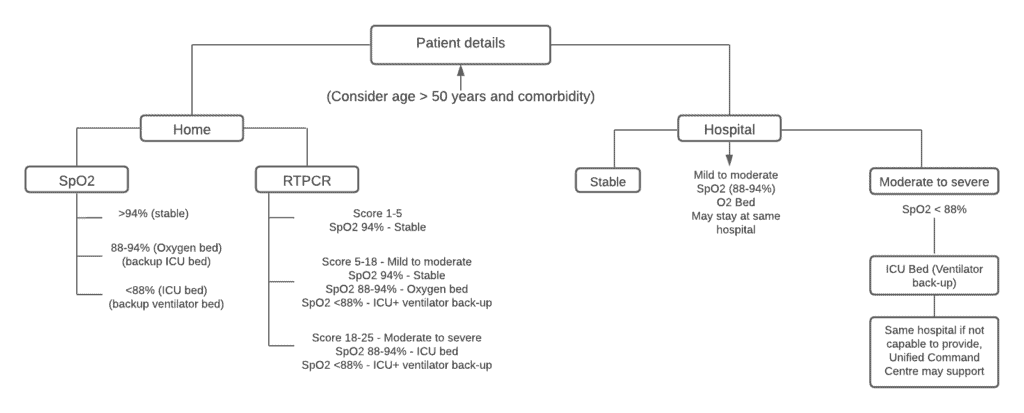
The exclusive tele-triaging wing with five doctors per shift is in-charge of COVID patients who develop serious symptoms and may need to be shifted to a COVID Care Centre or a hospital with oxygen beds.
“We attend to calls from various sources — 104, 191 and war room helplines — requesting for a hospital bed or other specific requirements. We talk to patients, assess their health status and prioritise their requirements based on a colour coding system,” says Dr B Ramesh, Trainee Medical Officer posted at the tele triaging department.
There are two colours in the triaging system — red (denoting ICU for high priority and emergency cases) and pink (denoting oxygen for moderate cases). The team coordinates with the bed allocation team from hospitals and care centres to allocate resources. Once the bed is reserved, the zonal team is alerted and an ambulance is sent to the residence of the patient.
“At our end, we ensure that we direct patients to hospitals that have vacant beds. As soon as we get a request, we share the requirements with the coordinator from our department, who then engages with the hospital and the patient. When there is no bed, the coordinator talks to the hospital staff and ensures that the patient is taken in. The hospital takes steps to stabilise the condition of the patient and makes arrangements to eventually get him admitted.,” adds Ramesh.
Explaining the challenges involved in the task, Ramesh adds, “The need for hospital beds peaked a few weeks ago and we were receiving a huge number of requests. We tried our best to get beds for patients from our side through coordinators. Our scope of work ends with informing the coordinator who then takes it forward with the hospital.”
Decentralised efforts
Besides the central war room set-up, the civic body has distributed the trainee medical officers across the zones of Greater Chennai Corporation to decentralise the efforts of the teams and identify critical cases and expedite their treatment.
The COVID war room set-up has been replicated in every zone of the city. The trainees have the contact numbers of the patients who are isolated at home. Each trainee has to follow up with anywhere between 50 and 90 patients per shift, depending on the caseload in their respective zones. Upon getting the medical history, they share the details with other volunteers designated to update the information on GCC’s COVID database.
“In the zonal headquarters, there is a teleconsultation team. I work in Zone 6 along with 25-30 doctors in my shift. Our job portfolio consists of following up on a COVID patient every two days,” explains Dr Jukhie Kamakshi Manghai, Trainee Medical Officer appointed on telemedicine duty.
The trainees start by asking the patients about 10 key symptoms of COVID that include fever, cough, breathlessness, loss of taste, loss of smell, body ache, vomiting and diarrhoea. They also check certain specific warning symptoms of serious illness, such as cough for five consecutive days and fever for seven consecutive days and signs of breathlessness.
“When a patient presents with any of the warning symptoms, we alert the Sanitary Inspector who immediately sends a fever survey worker and triaging team to the patient’s residence,” adds another Trainee Medical Officer from Zone 8. The norm is that a patient will be home-isolated for 14 days if they test positive with mild COVID. During that period, every patient will receive 5-8 follow-up calls.
“Decentralising the telemedicine strategy has reduced the burden on the health infrastructure. The dynamic nature of the new strain calls for patients to be on high alert. In our experience so far, we have realised that patients do not always pay keen attention to certain important and specific symptoms. Telemedicine facilities in every zone has made it possible to track every patient closely and notify the hospitals immediately if they develop any of these,” adds the officer from Zone 8.
Although the helplines were rolled out to handle COVID calls, the students on duty do receive non-COVID calls as well. “We have received calls from patients with diabetes and hypertension. In such cases, we direct them to the nearest diagnosis centre to take a test and depending on the results, we prescribe them tablets,” adds Pavithra.
COVID has also taken a toll on everyone’s mental health. Grief counselling for families of the deceased has proven to be a challenge. “We have had family members call and take out their angst on us. These are challenging times, we try our best to counsel and help them deal with the loss,” adds another officer from Zone 8.