If “vomiting” is the first remedial action that strikes you in an imagined event of poisoning, it may not be the correct approach in most cases. So, what is to be done if somebody ingests poison unknowingly or intentionally? Unfortunately, there is not much awareness of what constitutes poisoning and the correct response to it among the general public and even among doctors.
The World Health Organisation estimates that, in 2016, unintentional poisoning caused 106683 deaths and the loss of 6.3 million years of healthy life (disability-adjusted life years). According to a paper published in the Lancet Global Health in April 2017, poisoning accounts for 30% of suicides in India while accidental and environmental exposures to poisons are frequent.
The number of related incidents in India is not known as there is no central registry of poisoning cases. Developed countries have excellent reporting and recording systems with involvement of poisons control centres. While the mortality rate from poisoning in developed countries is estimated to be 1–2%, India reports a rate between 15 and 30%.
Though India has no national nationwide study on poisoning cases, one study, carried out in a tertiary care, teaching, public, urban hospital in Maharashtra and published in the Journal of the Association of the Physicians of India in 2019 found that mortality among 250 patients of poisoning was 24%. Common agents of poisoning were chemicals in 102 patients (41%), followed by pesticides (52 patients, 21%) and rodenticides (33 patients, 13%).
There are several misconceptions around poisoning. The usual response to this is to make the patients drink salty water to induce vomiting and in case of snake bite, even administer electric shocks. But experts say that none of this is the appropriate way to respond to a suspected case of poisoning. Which points to the need for setting up Poisons Information Centres whose staff will be able to tell callers what needs to be done.
Read more: Here’s what to do when you see a snake
The information gap
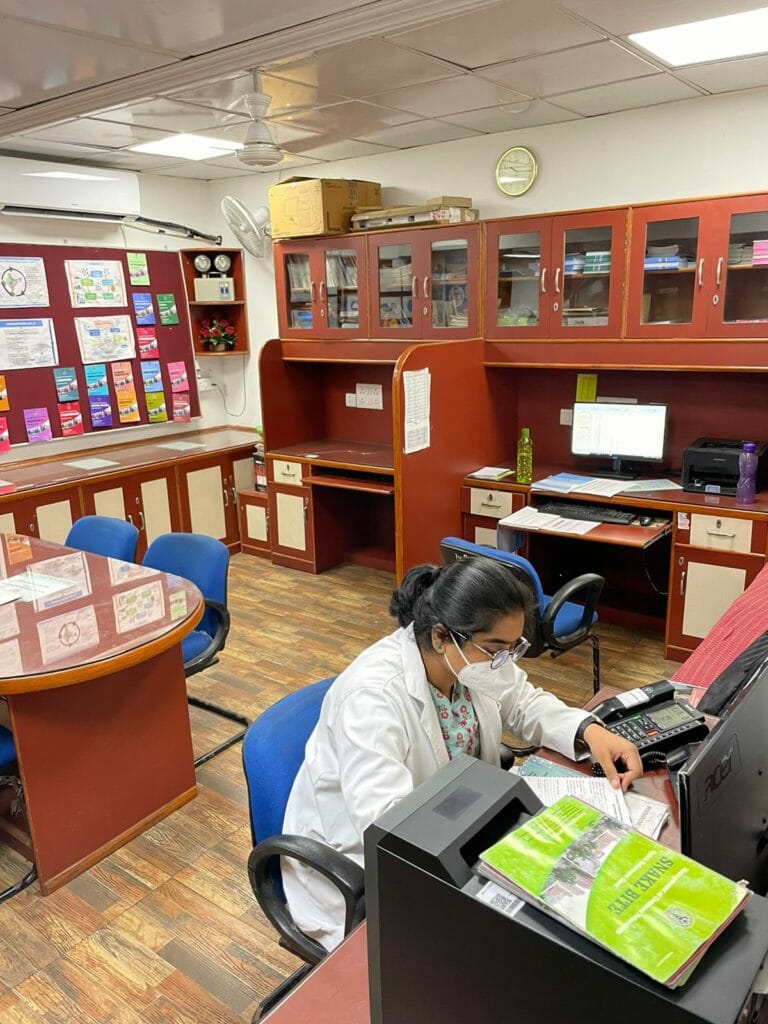
Poisoning is an emergency situation and needs specialised care and advice. Therefore, a system to provide adequate information to those in need is crucial. And that is what the relatively less-known National Poisons Information Centre (NPIC) at the All India Institute of Medical Sciences, Delhi is meant to do.
NPIC is the country’s first centre engaged in providing information on poisoning. Established in February, 1995 in the Department of Pharmacology at AIIMS, the centre provides toxicological information and advice on the management of patients suffering from exposure to or ingestion of poison. The centre has a continuous and systematic data collection system on poisons and drug reactions.
Since poisoning often happens due to lack of awareness, NPIC has initiated an awareness programme for educating school children, parents and occupational workers (lead acid battery manufacturing/recycling workers for example). The programme is being supported by the Department of Science and Technology.
The project with the theme “Be Cautious, Be Poison Safe” also proposes to introduce a ‘Poison Prevention Awareness Day’ for the first time in the country.
Poison centres in the country at present
Poison centres are sources of specialised expertise on diagnosis and management of poisoning, and toxicological research. Most centres provide emergency advice to the general public as well as to health professionals. The first poison information centre was set up in 1949 in the Netherlands.
India has less than 10 poison centres including the one at AIIMS, according to a list, including a map, of poison centres put out by the WHO. The US has 55 poison centres and a toll-free Poison Help line, which connects one to a local poison centre. “More than 70% of people who call a poison centre get the help they need over the telephone without having to go to a doctor or the hospital,” says the US’ Health Resources and Services Administration (HRSA).
Common incidents
“The centre gets 25-30 calls daily,” says Dr Swati Sharma, department of pharmacology at AIIMS and a scientist at the NPIC. “The centre has one toll free number and two landline numbers. We work 24 hours, all seven days of the week.
National Poison Information Centre: Contact numbers
Landline numbers: 011 26589391 | 011 26593677
Toll free number: 1800116117
Source: https://www.aiims.edu/
“Earlier, almost 80% of the calls used to be from Delhi, but now the centre gets calls from all over the country, even from Leh, Ladakh, Jammu and Kashmir, and north eastern parts of the country. Calls are mostly from doctors, parents and at times children. Sometimes people just call to check whether the centre is functioning. All the details of the caller are recorded”.
Dr Sharma was fielding calls even as I was talking to her. “Just now there was a call from a doctor, who consumed aftershave and was asymptomatic,” Dr Sharma said as an anecdotal example of how the centre works. Each call will require a different response depending on the patient and cause, she added.
The maximum number of calls relate to accidental or deliberate consumption of household items such as hand sanitisers, floor cleaners, antiseptics, mosquito repellents, pesticides, naphthalene balls, perfumes and even toothpastes. Advice is given according to the nature of poisoning and symptoms, Dr Sharma explained.
An analysis of telephone calls received by the NPIC from April 2006 to March 2016 revealed high incidence of poisoning, over 45%, from consumption of household products, followed by pharmaceuticals, agricultural pesticides and industrial chemicals. Among household items, household pesticides were commonly implicated, followed by household cleaners, thermometer mercury, naphthalene balls, antiseptics, kerosene, and paint thinner. Products such as camphor, silica gel, hair dye, nail polish remover, cosmetics, adhesives etc were also involved in some cases. The findings of this analysis of calls to the centre over a 10-year period was published in the Journal of Forensic and Legal Medicine.
Data subsequent to 2016 is being collated for publishing.

Risky home habits
Cases of poisoning have been increasing in the recent past. “During the lockdown, we were expecting fewer cases; however, the cases increased,” Dr Sharma said. “The number of calls from teenagers has also gone up”.
In children, poisoning is usually accidental and preventable. It happens largely due to negligence. Poisonous substances must be kept out of the reach of children who also need to be told repeatedly not to touch such substances. “For example, commonly used mosquito repellents are very attractive for kids due to their smell and the light blinking in the dispensers,” says Dr Sharma. “These must be kept at a height and completely out of reach of children. Parents should be watchful”.
Read more: Poisonous plants in gardens and homes
Another common practice in Indian households is to store potentially poisonous substances in containers different from their original ones, like keeping kerosene in a bottle meant for water, which has actually resulted in cases of poisoning. “Even adults can be confused and be poisoned accidentally,” says Dr Sharma.
One needs to be particularly watchful of labels as households keep non-consumable items like an antiseptic solutions next to consumable items like mouthwash. “Once we got a call from a physician who consumed hand sanitiser accidentally,” says Dr Sharma. In fact, since the COVID pandemic, there have been numerous cases and queries related to poisoning from consuming hand sanitiser.
MBBS education also needs a relook
“Medical education on poisoning too needs a re-look,” says Dr Narendra Nath Jena, President, Indian Society of Toxicology and director of Institute of Emergency Medicine, Meenakshi Mission Hospital and Research Centre, Madurai. “There is a need to upgrade the MBBS curriculum. Currently, even doctors do not know much about poisoning”.
Poisoning is a specialised area and needs dedicated education and training. say experts. The syllabus of toxicology in the MBBS curriculum does not incorporate enough knowledge on this subject. Currently, poisoning is taught under Forensic Science and toxicology.
There is a need to make the curriculum more elaborate and impart better teaching in clinical aspects of the subject. Doctors, nurses, paramedical staff, all need training, says Dr Jena.
What to do in cases of suspected poisoning
“People should not panic in case of consuming any poisonous substance,” says Dr Sharma. “One should also not induce vomiting, especially in case of poisoning by acidic or corrosive substances. The patient should get expert advice, and if needed rushed to a doctor or hospital emergency care. They should also not eat or drink anything after exposure.”
“While India reports a large number of deaths due to poisoning, we do not have an integrated programme on poisoning control and treatment,” adds Dr Narendra Nath Jena, President, Indian Society of Toxicology and director of Institute of Emergency Medicine, Meenakshi Mission Hospital and Research Centre, Madurai. “There are very few poison information and treatment centres.”

A state level poison information centre is being set up by the Tamil Nadu government. Dr Jena, who is involved in developing this centre, said all medical colleges should have poison centres for treating patients, and each state should have one helpline number assigned for poisoning related information for those in need.
Dr Jena says poisoning cases, both intentional and unintentional, are increasing. “My hospital gets one-two poisoning cases every day and I get 3-4 calls every day on my number,” he said.
Dr Jena added that poisoning as a subject also needs research, especially in the area of snake bites given that India is home to 50-60 poisonous snake species. “The public needs to be educated so that they do not go to quacks”.