India is in the grip of a second wave of COVID-19. What’s more, a new double mutated strain of SARS CoV2 has been detected. This is in addition to the Brazilian, South African and the UK strains. Reports of re-infection and positive cases among vaccinated people are coming in from various parts of the country.
The new strain(s) are more infectious and affect a younger population. Cases of children being infected are being recorded. Ominously, the new COVID cases may not be detected by routine RT-PCR tests. The R-value is increasing (R-value is the reproductive value which indicates how many others a positive person may infect)
How to protect oneself
Deploying the four-step strategy of PDII is the best known way of protecting oneself from COVID.
- P – Prevention
- D – Detection
- I – Isolation
- I – Intervention
Prevention
- Stay indoors as much as possible. If you need to step out, either opt for double masking (cloth + surgical mask) or an N95 mask
- Social distancing: keep a minimum distance of 6 feet from others. Avoid unventilated places.
- Scrubbing: wash your hands regularly.
- Shielding: do not touch your face when you are in public.
Detection
Pay attention and catch symptoms early. With mutations of the virus, the symptoms are also expanding.
Get an RT-PCR test done.
Last year’s symptoms: Dry cough, fever, weakness, breathing problems, loss of smell/taste.
New symptoms: Apart from above, any of the following symptoms could be present:
- Headache
- Mild diarrhea
- Body ache
- Weakness
- Uneasy feeling
- Vomiting
- Hearing problems
- Conjunctivitis
- Myalgia (muscle pain)
Isolation
At the onset of symptoms, the patient should be isolated in a well-ventilated room with an attached bathroom, so that she does not have to step out for 10 days.
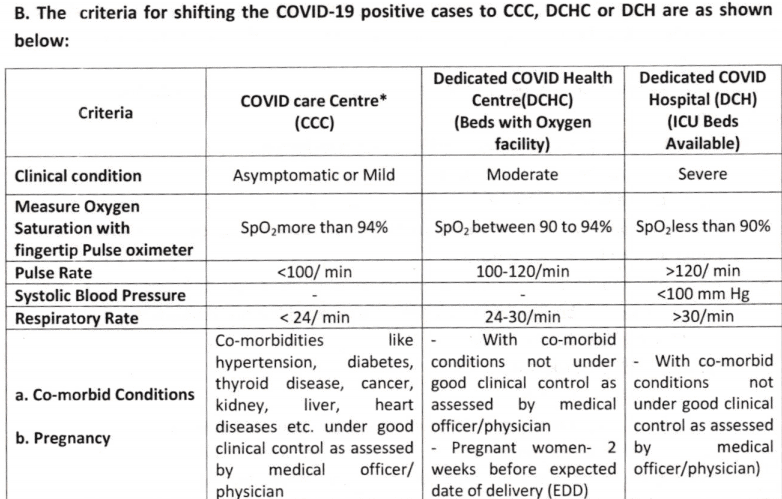
The Karnataka government’s guidelines — through its circular dated 20.04.2021 — specifies what makes a patient eligible for home isolation/home care, and also the criteria to be used for shifting the person to a CCC (COVID Care Centre), DCHC (Dedicated COVID Health Centre) or DCH (Dedicated COVID Hospital).
Eligibility for home isolation
- Patient should be clinically assigned as an asymptomatic/mild case through telephonic triage or by the health staff/medical officer/physician.
- Has mild fever < 38 deg C (< 1OO.4 Deg F)
- Oxygen saturation should be >= 95%
- Elderly patients aged more than 60 years and those with co-morbid conditions such as hypertension, diabetes, heart disease, chronic lung/ liver/ kidney disease, cerebrovascular disease, etc. shall be allowed home isolation/home care only after proper clinical evaluation by the treating medical officer/physician/ family doctor
- Patient should have the requisite facility at their residence for self-isolation and also for quarantining family contacts
- A caregiver should be available to provide care on a 24 X 7 basis
- The patient should provide a signed undertaking for self-isolation/home care and follow guidelines of home isolation/home care
Exceptions
- Home isolation/home care shall not be applicable for pregnant women two weeks before the expected date of delivery.
- If symptoms increase in the next 12-24 hours, the patient must be shifted to CCC/DCHC depending on the situation
- When the house is not suitable for isolating the patient at home
- Shifting of the person may also be considered if the asymptomatic person opts for CCC.
Intervention
Timely medical intervention
Monitoring COVID-19
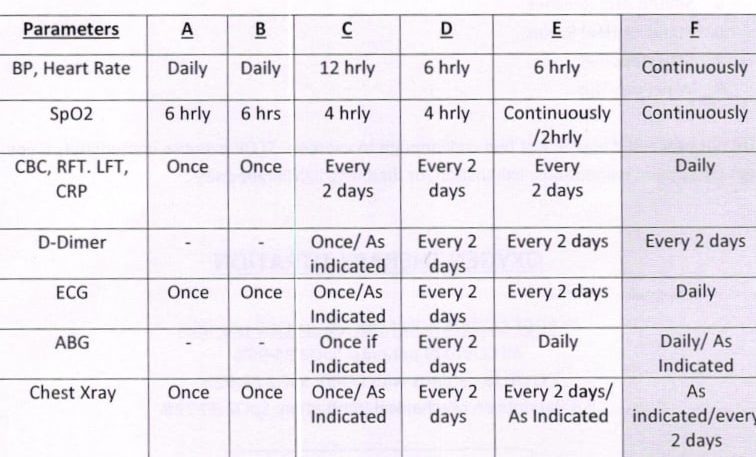
4.0) dated 20.04.21
*Parameters : A & B – Home Isolation **C to F is part of the institutional care approach
If you test positive, keep these handy:
Information
1) Contacts of family doctor/neighbourhood doctor, RWA office bearers/local volunteers
2) Contact numbers of COVID helpline of your district, district hospital, ambulance, medical store, medical oxygen cylinder provider, local plasma bank, people who have recovered recently from COVID-19, private and government COVID-19 testing labs servicing your area.
Documents
1) Insurance details, medical records, list of allergies, etc.
2) Form for COVID testing: Spare copies with data filled for everybody, to save on exertion when you are sick
3) Home isolation declaration, printed, with a few spare copies and extra blank sheet
Other Items
1) Finger pulse oximeter with spare batteries. Epidemiologist Rifa Khan suggests procuring one per family, or the local RWA or apartment association could keep a few stocked.
2) Face masks, thermometers, regular medicines
3) Toiletry and sanitation kit
4) Water bottle and cutlery (for use during quarantine), electric kettle and electric steamer
5) Garbage bags for proper disposal of trash
6) Large can of Sodium Hypochlorite or a disinfectant like Lizol, and hand sanitisers
7) Mobile charger, cable, power bank, laptop
8) Cash, credit card, cheque book, banking details, etc. for payments at the hospital
9) Bag: Comfortable clothes for the duration of stay.
Discharge protocol after home isolation
Patients under home isolation will stand discharged (released from home isolation/ home care) after 10 days of symptom onset (or date of sampling, for asymptomatic cases) and no fever for three days. Thereafter, the patient is advised to isolate at home and self-monitor their health for a further seven days.
They shall be released if the following criteria are met: .
- No symptoms
- No fever (recorded body temperature < 37.5 deg C or <99.5 deg F )
- Maintains oxygen saturation above 95%
- Respiratory rate less than 24 per minute
There is no need for any COVID-19 test (RT-PCR/CBNAAT/True-NAT/Rap|d Antigen test) after the period of home isolation/home care is over. The person is allowed to resume work only after satisfactory completion of home isolation/ home care.
A fitness certificate would be issued by the concerned area medical officer (PHC/UPHC/CHC/GH )/ treating physician/ family doctor. Alternatively, an e-certificate may be issued in the prescribed format by the tele-monitoring team.
Emergency Contacts
BBMP Covid Helpline Number: 1912
For queries and advice, call Apthamitra: 14410
Emergency cases, ambulance, hospital transfers: 108
State War Room: Corona Positive / Test Information
BBMP portal: Covid+ Hospital Bed Management Status-CHBMS
BBMP Zonal Helpline numbers
| East Zone | 7411038024 / 9886496295 |
| West Zone | 080-68248454 |
| South Zone | 8431816718 |
| Mahadevapura Zone | 080-23010101 / 080-23010102 |
| Bommanahalli Zone | 8884666670 |
| Yelahanka Zone | 9480685964 |
| R.R. Nagar Zone | 080-28601050 |
| Dasarahalli Zone | 080-29590057 / 080-29635904 / 080-29635906 |
Strict adherence of COVID appropriate behavior such as wearing a mask, hand sanitisation and social distancing, is a must. Besides these, vaccination is the key.
Thanks. Very useful information. You could also add Bangalore Covid helpline number 080-47190606. Very responsive.
very explanative danyavadamulu