On June 27, Bengaluru’s National Institute of Mental Health and Neurosciences (NIMHANS) formally launched its digital academy, virtually, with the government’s participation. Along with NIMHANS director B.N Gangadhar, who was at the office of the Union Health Minister JP Nadda in New Delhi, 500 doctors from 15 states logged in.
“It was a formal event. We announced the course, launched digital books and shared the link to the website. We also discussed the agenda, and the benefits of distance education in this sector,” Gangadhar said.
Mental illnesses present an ever-growing cause for concern across the world. Statistics that emerge from World Health Organization (WHO) studies and psychiatrists from around the world continue to shock, and indicate the rise of mental health problems across age groups and economic backgrounds. The reality in India is no less alarming.
According to the National Mental Health Survey conducted in 2015-2016 in 12 states, 10% of Indians currently suffer from common mental health disorders and 12.3 of Indians are affected at some point in their lives, but these go largely untreated. This statistic is reflected in the number of patients seeking treatment at NIMHANS, and its rise year on year. 2017 saw the number of people seeking help at the Institute rise to 550,500 from 500,000, thus accounting for a 10% rise in footfalls.
Director B.N Gangadhar confirmed the statistics but is wary of the assumption that this is due to an epidemic of mental illnesses within a specific or predetermined time frame, as there is no specific study to back such a claim. He is more concerned with the knowledge gap that leads to the spread of false alarms.
“It is unfair to place the burden on psychiatrists alone, especially to deal with common mental disorders, such as insomnia, depression, anxiety and substance abuse. Common mental disorders, earlier classified as minor disorders, affect 80% to 90%, or nearly 13 crore of the 15 crore sufferers of mental health problems in our country. It should be as simple as approaching a general physician for a headache. The doctor should also be able to diagnose a common disorder and solve the issue faster,” said Gangadhar.
The need for a digital academy
The National Mental Health Survey 2016 pointed out existing gaps in treatment for common mental health disorders in the states of Punjab, UP, Tamil Nadu, Kerala, Jharkhand, Gujarat, West Bengal, Rajasthan, MP, Chhatisgarh, Assam and Manipur. It inferred that for common mental health disorders, there was an 85% treatment gap across the states.
This prompted NIMHANS to start the process of teaching general physicians how to identify and deal with such patients, and tackle common symptoms such as lack of sleep, irritability and depression.
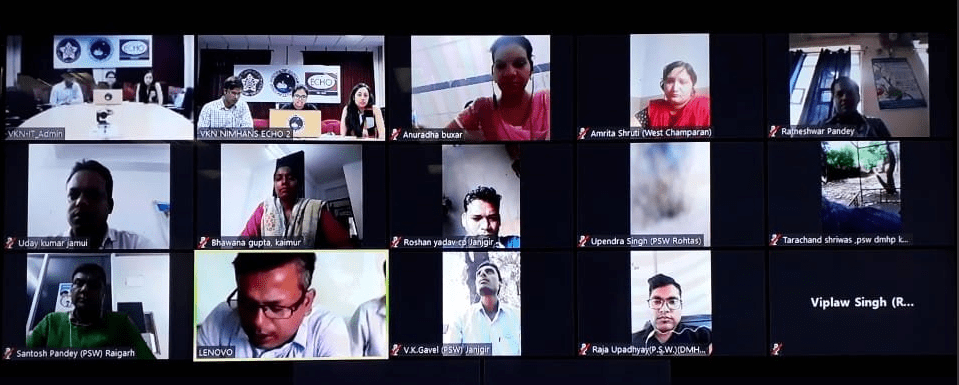
“It becomes difficult for people staying in rural or remote areas to travel to the community centres and avail the right treatment for psychological well-being. Hence we want to use the power of ‘digital’ in helping them, while educating the doctors, ‘ said Dr Prabhat Chand, the team leader and coordinator of the Virtual Knowledge Network. Practitioners can tune in through their mobiles from Android or iPhone platforms.
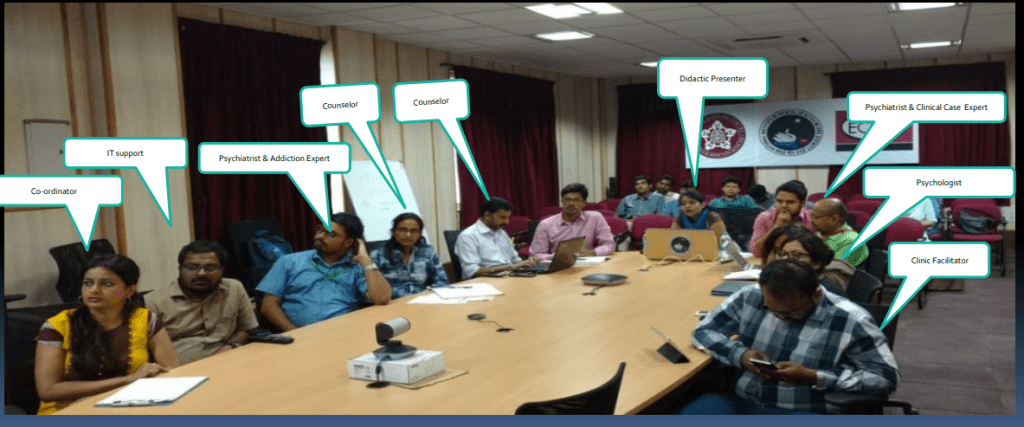
Psychiatrists, doctors, social workers and counselors sit down together to conduct a teaching session for doctors across the country. Pic Credit: NIMHANS
States keen on digital education
The idea of the digital academy received further boost due to the demand and interest shown by nodal health officers, who have been striving to find the fastest and cheapest routes to curing rising psychological problems among the populace in the respective states. Doctors from Gujarat, Orissa and Maharastra are currently waiting to get started with the digital training program.
Every year Niti Aayog hosts a health conference in different parts of the country with health secretaries of 28 states to discuss solutions for the health sector. The team in NIMHANS headed by Prabhat Chand made a presentation titled ‘Innovative Public Health Model’ at Thirupathi in 2016.
“The presentation illustrated the hub and spokes model that could be applied to teaching them. Since it was low-cost, health secretaries from Bihar, Chhattisgarh and Uttarakhand, immediately came on board to start the process of educating their doctors in the field of psychiatry.
In Bihar, many MBBS level doctors applied on their own, just out of the love of learning. “The sessions mainly dealt with addiction-related problems, as Bihar has had a problem with high levels of alcoholism,” said Chand.
“A corpus fund was proposed with Rs 30 lakh allocated to hire a team of four ( 1 doctor, 1 nurse, 1 social worker and counselor) teaching and training, but now the money is being taken out of the annual expenditure given to NIMHANS by the government,” explained Gangadhar.
Hub and Spokes model
So, what exactly is this hub and spokes model all about?
Within the vast NIMHANS campus, Virtual Learning Centers along with telemedicine facilities are already in place, where different courses are conducted on a weekly basis for doctors and social workers who treat addicts in Bihar and Uttarakhand. Now, it will expand to start reaching out to doctors without specialization in psychiatric care across the nation. A NIMHANS-accredited certification of Diploma in Community Health will be awarded with alternative specializations in counseling, nursing or psychiatry.
An ongoing ‘Hub and Spokes’ discussion. Pic: NIMHANS.
The team conducting such sessions will be multi-disciplinary, and the sessions themselves will be interactive, with the GPs also getting a chance to present scenarios from their side. The training will involve discussions on real and hypothetical cases, along with the appropriate measures to be taken in such cases.
Once the primary health care doctor sends the details of a case being treated (three days before the weekly meeting), the hub experts compile their advice and put it across. At the end of the session, they generally have a theoretical summary as per the module. Both pre-recorded self-based learning and live interactions are available to the attendees.
The course is divided into four modules.
- Communication skills
- Depression and Anxiety
- Psychosis
- Intervention
“Earlier, virtual courses were handled by in-house NIMHANS psychiatrists, but now they have recruited a dedicated team to solely handle the teaching in such courses, as demand has increased,’ said Prabhat Chand. On a daily basis, we have 50 people in a batch, who take turns to speak and clear their doubts at the end of each session. If the MBBS level doctor has a doubt, it is cleared with a psychiatrist, and if a nurse raises a question, it will be answered by a nurse,” explains Prabhat Chand.
A successful case: Karnataka State Tobacco Control Programme
In 2016, the nodal officer in the state Tobacco Control Programme approached NIMHANS to train their social workers. They came over to the Institute from 16 districts in Karnataka for only a day for on-sight training, as the funding was limited. After going back, they logged on to online sessions to learn how to treat tobacco addicts with psychological expertise. Within six months it increased their success rates.
Traditionally, graduates in social work, sociology and the humanities would deal with tobacco consumers, but were still unable to get through to them. Digital teaching helped disseminate the specialised knowledge needed to counsel addicts.
“The virtual knowledge network through its hub-and-spokes model developed by the team at NIMHANS has trained and mentored over 3000 health professionals. The trained professionals include counselors, private health care providers, physicians, psychiatrists, residents, and community workers. Through them, over 30,000 patients in remote areas have been provided mental health care more effectively. People from very remote parts of the country have been able to join the programme through a simple smart phone, presented their clinical cases and sought help to effectively manage these cases,” reads a statement put out by NIMHANS.
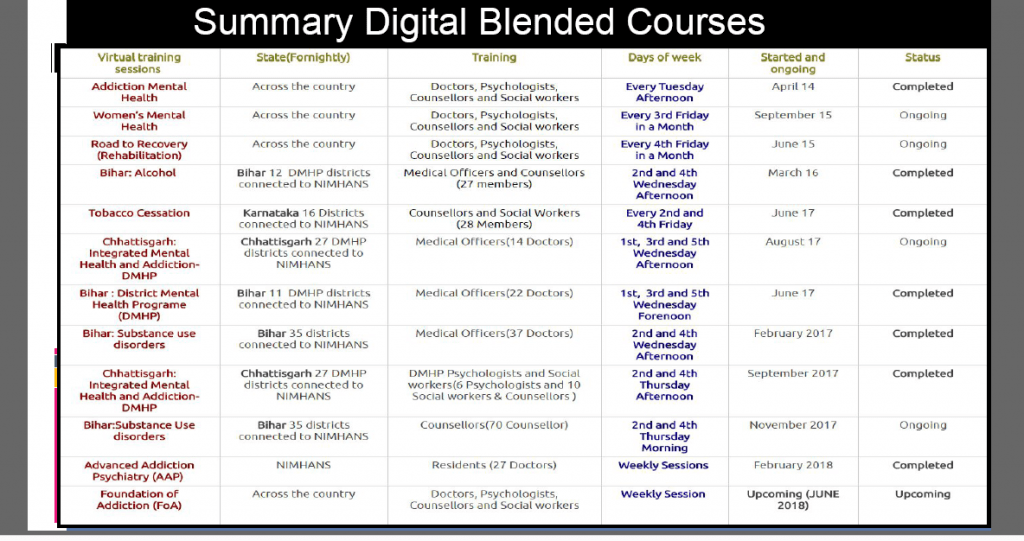
Number of courses that are ongoing and completed by the NIMHANS digital academy.
Now, with the formal launch of the digital academy and general physicians also brought into the fold of trainees in courses offered, the reach of mental health care in the country is expected to rise significantly.
Infrastructure expansion
Apart from expanding digital education, Gangadhar said that 125 beds and three more operation theatres will be added to the neuro-surgery department, especially to cater to the difficult cases that are being referred to the hospital increasingly.
One of the reasons for the high number of referrals to NIMHANS is, of course, the strength of the Institute’s research in specific areas, and medical expertise for cases which are difficult to diagnose. Eight hundred research papers were published in the last financial year alone, which were all peer-reviewed and published in Indian scientific journals.
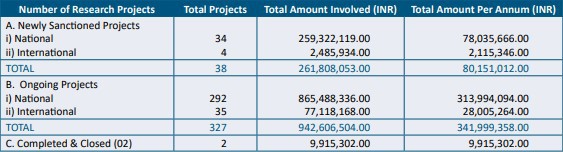
Studies taken on by the Institute in the year 2015-16. Source: The annual report of NIMHANS (2015-2016)
“There has been a 40% increase in complicated cases such as epilepsy, muscular dystrophy and brain tumours referred to NIMHANS for surgeries and also research that could yield unique medical solutions. Three more operation theatres are currently being built to effectively deal with these, as currently only 7 out of ten operation theatres are functional,” he said.
Another 125 beds are being added to the general ward, where follow ups and overnight care are required. The first set of 125 beds were added in June to the neuro-surgery ward, and the next expansion is set for the month of July.