On 27th April 2021, the COVID figures released by Municipal Corporation of Greater Mumbai (commonly referred to as MCGM or BMC) showed the count of positive patients in the city at 66,045.
The positivity rate in Mumbai stands at over 13% which means that approximately 1 out every 8 people getting tested is infected with the virus. Though numbers have been falling over the past week, Mumbai continues to be the worst-affected in Maharashtra. Newer hotspots in the Mumbai Metropolitan Region such as Kalyan-Dombivli, Thane, and Navi Mumbai, are mushrooming. The government is struggling to ramp up health infrastructure even as complaints of lack of ambulances, beds, and other health facilities mount.
When to worry
When you feel symptoms, ISOLATE immediately so that you do not spread the virus, if you have it.
The symptoms in the second wave are not all the same as those of last year. Here is a list, though not exhaustive.
Last year’s symptoms: Dry cough, fever, weakness, breathing problems, loss of smell/taste.
New symptoms: Headache, mild diarrhea, body ache, weakness, uneasy feeling, vomiting, hearing problems, conjunctivitis, myalgia (muscle pain).
If any symptoms persist for 2 days, one should contact a healthcare professional and get checked. Do not ignore such symptoms and wait for more than 3 days. It will be helpful to track the oxygen levels, twice a day with the help of a pulse oximeter, especially for elderly and those with comorbidities.
Here’s a step-by-step guide on what to do if you feel ill and suspect COVID-19 in Mumbai:
In order to compile this guide, we talked to people who had COVID cases in their families and also called the Ward A and B War Rooms where the operators transferred the call to in-house doctors, Dr. Dhananjay More and Dr. Aafraa Seth, who clarified the whole process.
Step 1: Getting a COVID test
Call up your Ward War Room number for testing assistance OR arrange for a test on your own.
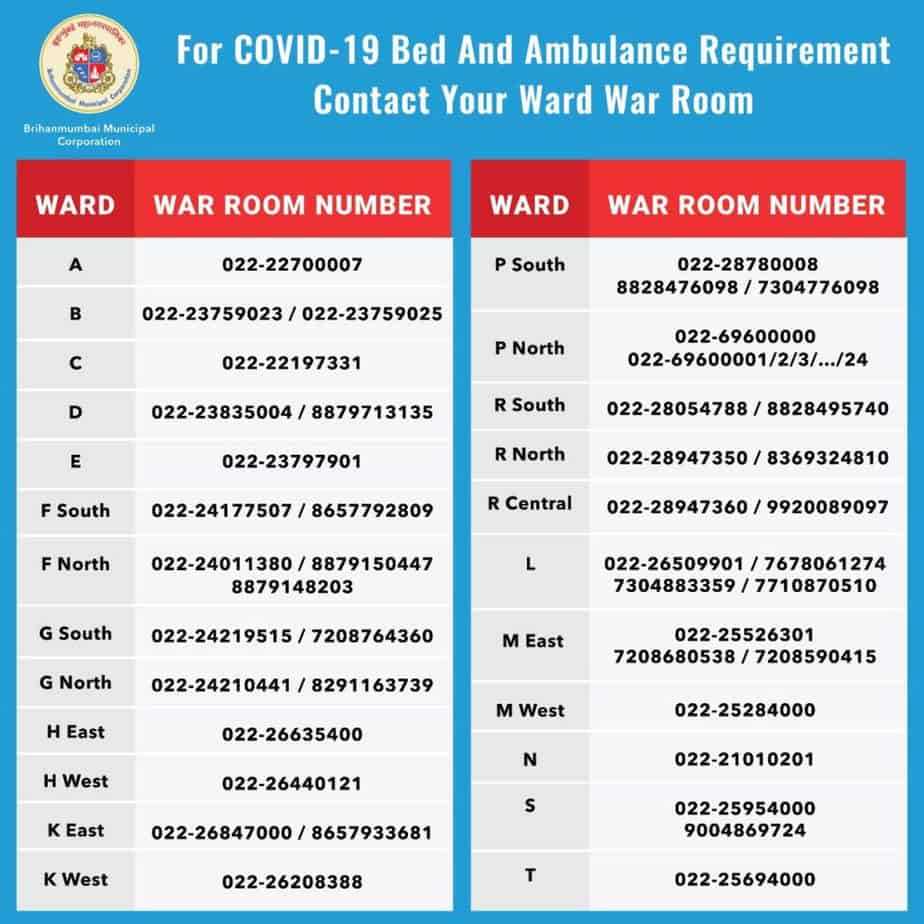
The corporation recently revamped the control rooms as Ward War Rooms for the city’s 24 wards. You can call your Ward War Room for assistance with identifying your symptoms. [The operators also help with information on where to get tested, identifying a vacant hospital bed or coordinating ambulance services.]
Where to get tested?
All laboratories are required to submit COVID test reports to Indian Council for Medical Research (ICMR) – so you can get tested at any laboratory. Some labs offer home collection of samples. For free testing, there are health posts set up in every ward where you can get tested after showing your Aadhar card. To find out the locations of the health posts in your ward, contact the War Room.
Which test to do?
- Two tests are being done. In both, healthcare professionals take a throat or a nasal swab to detect the presence of a virus.
- The Rapid Antigen Test (RAT) uses a home-pregnancy type of kit. It is quick and results show in about 15 minutes.
- The Reverse Transcription Polymerase Chain Reaction (RT-PCR) test is said to be more conclusive. Results come in about 24 hours.
- If you don’t want to wait for the RT-PCR test results (especially if you are symptomatic), you can get a RAT done and if that’s positive, it is likely that the RT-PCR will be positive too.
What are the costs?
The cost of testing is free in Municipal Health posts. On 1st April, 2021, the Maharashtra State Government capped the charges at Rs. 500 for an RT-PCR test at the collection centre and Rs. 800 for home collection. For RAT, the price is fixed at Rs. 150 and Rs. 300 respectively.
Step 2: What happens if you test positive
If a person is positive in the Rapid Antigen Test he/she will be treated as per protocol mentioned below, or, if not showing symptoms, may be asked to undergo an RT-PCR test for confirmation.
If a patient tests positive in the RT-PCR, then ICMR, BMC and the patient are informed. The patient should expect a call from BMC after testing positive.
On 24th April, 2021, BMC released revised guidelines and hospitalisation protocol, to ensure effective bed management. At the first level, you and your housemates will necessarily have to home isolate/ quarantine. Depending on your physical condition, it will be decided whether or not you need hospitalisation.
Prior to the new guidelines, patients were allowed for home isolation, subject to certain conditions. While these do not apply currently, it makes good sense to follow them to the extent possible.
- The patient should have a separate well-ventilated room with a separate toilet.
- The patient shall stay in the identified room and away from other persons in the home (especially the elderly and those with co-morbid conditions like hypertension, cardiovascular disease, renal disease, etc.).
- The patient must have a pulse oximeter, digital thermometer, face masks, gloves, sanitiser, etc. to be used during home isolation.
- The patient shall report to the IVR call/health staff /medical officer/family physician about their health status and maintain the chart of vital parameters at home.
- The release of the patient from home isolation shall be as per the existing discharge protocol of the state for COVID.
- The home isolation shall be with the knowledge of the family members, neighbours/society, treating physician and local Health Posts.
When at home, follow the medication and regimen given by your doctor. Check oxygen 3-4 times a day. SpO2 of less than 94% on the pulse oximeter (given 2% margin of error, it means low of 92%) would require medical attention.
You may be advised to do blood tests such as CBC (Complete Blood Count), CRP (C-Reactive Protein) and D-Dimer or a CT-Scan. These are to determine the extent of infection and severity. To get these done, you will have to step out of your house. Be double-masked, wear gloves, and inform the lab/hospital that you are COVID positive.
Difference between Quarantine and Isolation
- Isolation is used to separate ill persons who have a communicable disease from those who are healthy. Isolation restricts the movement of ill persons to help stop the spread of certain diseases. For example, hospitals use isolation for patients with infectious tuberculosis. Same applies for COVID.
- Quarantine is used to separate and restrict the movement of apparently healthy persons who may have been exposed to a communicable disease to see if they become ill. These people may have been exposed to a disease and do not know it, or they may have the disease but do not show symptoms. Quarantine can also help limit the spread of a communicable disease.
If you test negative
If you have symptoms but your tests have returned negative results, continue to take precautions. There have been cases where RAT and RT-PCR give negative results but oxygen levels kept dropping. Isolate and regularly check your pulse and oxygen levels.
Step 3: If you need hospitalisation
At the time of detection of COVID, symptomatic patients who need hospitalisation are allocated a hospital bed after examination by BMC medical staff at the patient’s home. In case of emergencies, BMC may make exceptions.
All bed allocations are done only through the War Rooms.
Read more: BMC guide to getting a COVID bed in Mumbai
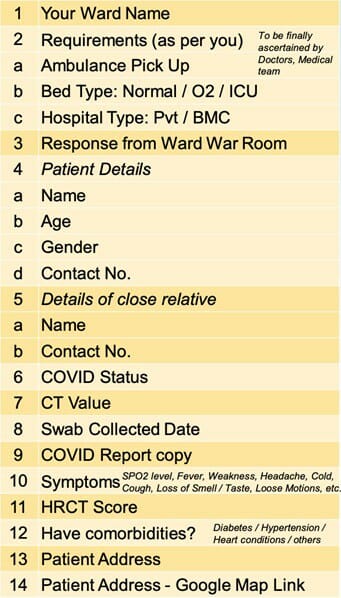
This is the basic information to be kept in handy when you call the Ward War Room for admission into a treatment facility:
When you feel the need for hospitalisation, the operator at the Ward Control Room will note your requirement and call the nearby hospital to confirm the availability of a bed. “We call and confirm because we don’t want that bed to be claimed by another patient,” Dr Wakshe says. The operator also has numbers of ambulance drivers to coordinate the ambulance service. Depending on the severity of the condition, they might arrange an oxygen bed or a ventilator bed.
According to data on the BMC dashboard on 26th April, 2021, BMC has a bed capacity of 29,903 of which 21,681 are occupied. Only 48 ICU beds and 23 ventilator beds are available and the rest are occupied.
The Maharashtra Government had capped charges for an isolation ward at Rs 4,000 a day, the maximum charge for an ICU was capped at Rs 7,500 a day, and charges for ventilators were capped at Rs 9,000 a day. These were the prices in Government hospitals as well as 80% of isolation beds in the private hospitals. Last month, the Maharashtra Government extended this 80:20 ratio till 31st May 2021. This means that all private hospitals will charge government rates for 80% of its isolation beds for COVID patients and the rest 20% can be charged as per their own rates.
What is the discharge policy?
There is no forthcoming discharge policy from the BMC. BMC had been following the ICMR discharge guidelines, according to media reports. Towards the end of March 2021, they decided to release asymptomatic patients to make space for moderate and severe cases.
Currently, as hospital beds are in high demand, patients who are on the road to recovery are being discharged and told to continue with home isolation at home.
Priyanka, a resident of Mumbai, whose mother recently recovered from COVID said that before discharge, blood tests like CRP (C-Reactive Protein) and D-Dimer were done. These were normal, so they released her mother as there were several patients in need of a bed. The RT-PCR test was not done.
Getting vaccinated after testing positive
If you have had COVID, you should wait 4-8 weeks after recovery from COVID symptoms before taking the vaccine. If you were treated for COVID with monoclonal antibodies or convalescent plasma, you should wait 90 days before getting a COVID vaccine. This also applies to those who have taken one vaccine dose and waiting to take the second dose.
Certain research studies suggest that those who recovered from COVID who haven’t been vaccinated as yet, should be fine with one dose, and not two.
Please do have your condition assessed by your doctor and vaccinate as advised.
For those who want to get vaccinated, the functional vaccination centres are announced every morning by BMC on Twitter https://twitter.com/mybmc.
Also read: